Acne is a common skin condition that affects millions of people worldwide, regardless of age, gender, or ethnicity. While it’s often perceived as a mere inconvenience, acne can significantly impact one’s self-esteem and mental well-being. Understanding the different types of acne is crucial for effective management and treatment. In this comprehensive guide, we’ll delve into the various forms of acne, their causes, symptoms, and treatment options.
I. What is Acne?
Acne, also known as acne vulgaris, is a skin condition characterized by the formation of pimples, blackheads, whiteheads, cysts, and nodules. These occur when hair follicles become clogged with oil and dead skin cells, leading to inflammation and bacterial growth. Acne commonly appears on the face, neck, chest, back, and shoulders, where sebaceous glands are most active.
II. Types of Acne:
- Comedonal Acne:
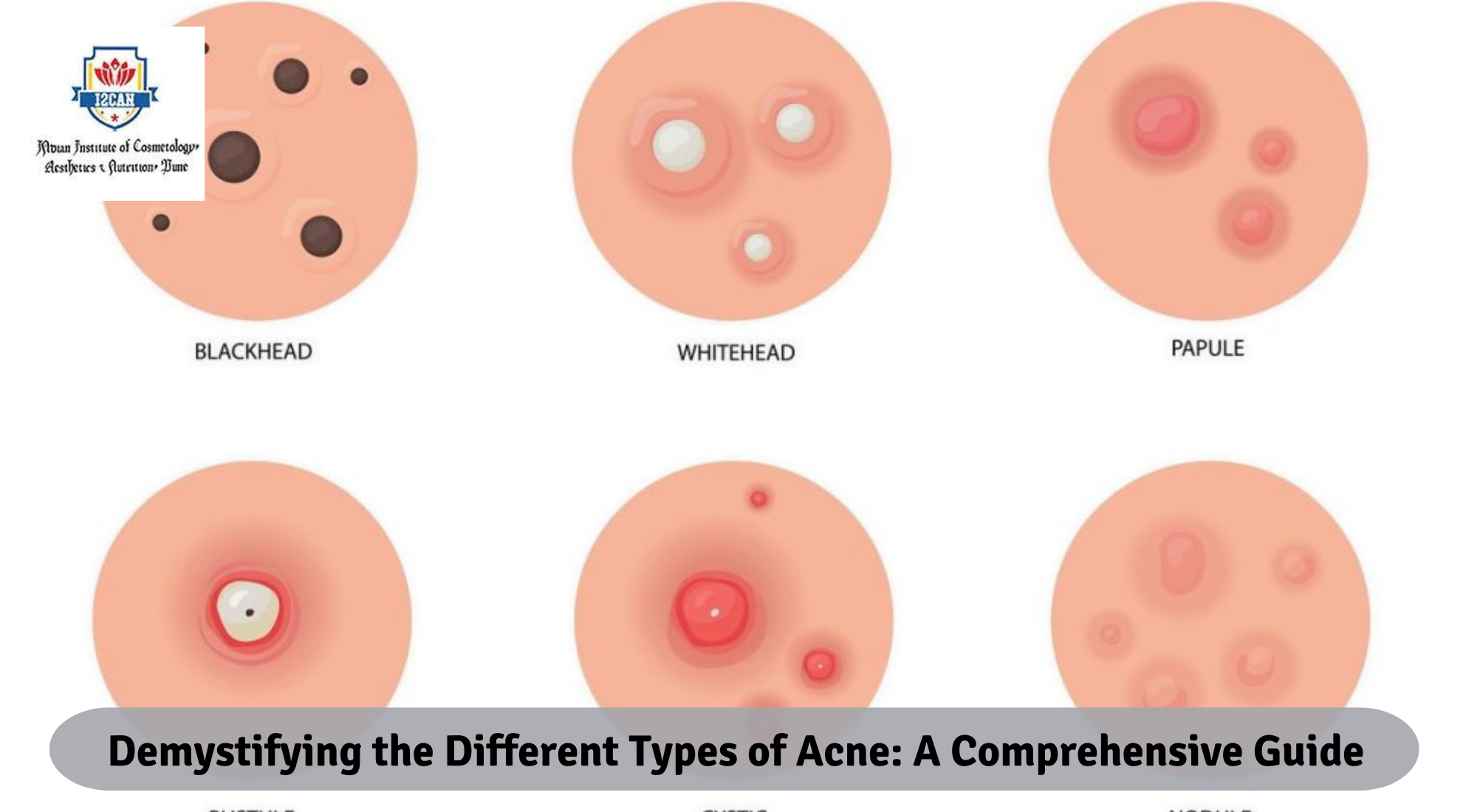
- Comedones are non-inflammatory lesions that include blackheads and whiteheads.
- Blackheads (open comedones) occur when pores become clogged with excess oil and dead skin cells, oxidizing and turning black upon exposure to air.
- Whiteheads (closed comedones) are similar to blackheads but remain closed under the skin’s surface, appearing as small, flesh-colored bumps.
- Inflammatory Acne:
- Inflammatory acne involves red, swollen lesions caused by bacterial infection and inflammation.
- Papules are small, red bumps that develop when the walls of hair follicles break down, leading to inflammation.
- Pustules are pus-filled lesions characterized by white or yellow centers surrounded by red, inflamed skin.
- Nodules are large, painful, solid lesions that form deep within the skin. They result from the buildup of sebum and bacteria, often requiring medical intervention for treatment.
- Cysts are similar to nodules but larger and filled with pus. They can cause scarring and require professional treatment to prevent complications.
- Acne Rosacea:
- Acne rosacea is a chronic inflammatory skin condition characterized by redness, flushing, and acne-like papules and pustules, primarily affecting the central face.
- It often occurs in adults and may be triggered by factors such as sunlight, stress, spicy foods, and alcohol consumption.
- Unlike traditional acne, acne rosacea typically lacks comedones but may involve ocular symptoms such as dryness, itching, and irritation of the eyes.
- Acne Fulminans:
- Acne fulminans is a severe, rare form of inflammatory acne that often occurs suddenly and aggressively in young males.
- It is characterized by the rapid onset of painful nodules and ulcerations, accompanied by systemic symptoms such as fever, joint pain, and malaise.
- Treatment usually involves oral isotretinoin (a powerful acne medication) and systemic corticosteroids under medical supervision.
- Acne Mechanica:
- Acne mechanica results from friction, pressure, or heat applied to the skin, leading to the development of acne lesions.
- It commonly affects athletes, military personnel, and individuals who wear tight-fitting clothing or equipment.
- Prevention involves wearing loose, breathable clothing, using non-comedogenic skincare products, and maintaining good hygiene practices.
III. Causes of Acne:
- Excess Sebum Production:
- Sebum, an oily substance produced by the skin’s sebaceous glands, plays a crucial role in maintaining skin hydration. However, excessive sebum production can contribute to acne formation by clogging pores and promoting bacterial growth.
- Clogged Pores:
- Dead skin cells and excess oil can accumulate within hair follicles, leading to the formation of comedones (blackheads and whiteheads). When bacteria proliferate within these clogged pores, inflammatory acne lesions may develop.
- Bacterial Overgrowth:
- Propionibacterium acnes (P. acnes), a type of bacteria found on the skin, can proliferate within clogged pores and trigger an inflammatory response, leading to the development of acne lesions.
- Hormonal Fluctuations:
- Hormonal changes, such as those occurring during puberty, menstruation, pregnancy, and menopause, can influence sebum production and contribute to acne flare-ups. Androgens, in particular, play a significant role in stimulating sebaceous gland activity.
- Genetics:
- Genetic factors can predispose individuals to acne by influencing sebum production, follicular hyperkeratinization, and inflammatory responses. A family history of acne is often observed in individuals with severe or persistent acne.
IV. Treatment Options:
- Topical Treatments:
- Topical treatments for acne include over-the-counter products containing benzoyl peroxide, salicylic acid, retinoids, and azelaic acid. These ingredients help unclog pores, reduce inflammation, and inhibit bacterial growth.
- Prescription-strength topical medications, such as topical retinoids (tretinoin, adapalene) and topical antibiotics (clindamycin, erythromycin), may be recommended for moderate to severe acne.
- Oral Medications:
- Oral antibiotics (tetracycline, doxycycline, minocycline) are often prescribed for inflammatory acne to reduce bacterial overgrowth and inflammation. However, prolonged use can lead to antibiotic resistance.
- Oral contraceptives containing estrogen and progestin can help regulate hormonal fluctuations and improve acne in women.
- Oral isotretinoin (Accutane) is a potent medication reserved for severe, recalcitrant acne that has not responded to other treatments. It works by reducing sebum production, shrinking oil glands, and preventing acne recurrence.
- Procedures:
- Dermatological procedures such as chemical peels, microdermabrasion, laser therapy, and photodynamic therapy (PDT) can help improve acne by exfoliating the skin, reducing inflammation, and killing acne-causing bacteria.
- Intralesional corticosteroid injections may be used to treat large, inflamed acne cysts and nodules by reducing swelling and promoting healing.
- Lifestyle Modifications:
- Adopting a gentle skincare routine involving non-comedogenic products and avoiding harsh scrubbing can help prevent further irritation and inflammation.
- Dietary modifications, such as reducing dairy consumption, limiting high-glycemic foods, and avoiding trigger foods, may benefit some individuals with acne-prone skin.
- Managing stress through relaxation techniques, regular exercise, and adequate sleep can help reduce cortisol levels and minimize acne flare-ups.
Conclusion:
Acne is a multifactorial skin condition that can manifest in various forms, ranging from comedones to severe inflammatory lesions. While genetics, hormonal fluctuations, and bacterial overgrowth play significant roles in acne development, effective treatment strategies often involve a combination of topical medications, oral therapies, dermatological procedures, and lifestyle modifications. By understanding the different types of acne and their underlying causes, individuals can take proactive steps to manage their condition and achieve clearer, healthier skin.